I propose looking at the "where is the $" question in three different areas:
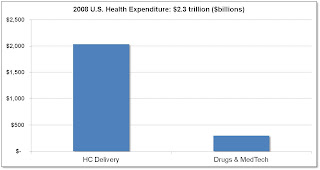
1. Hospital / Provider spending vs. Medtech / Pharma: Data shows that medtech / pharma constitute only 3% of overall healthcare spending vs. hospital / provider, which would lead to a conclusion that there may be more room for cost reduction in hospital / provider. This doesn't take into account, however, how medtech / pharma may be the driver for increased care. Here's the data:
Source: American Well: The Doctor Will E-See You Now HBS CASES | ELIE OFEK, RON LAUFER | MAR 30, 2010.
2. Chronic Disease: It makes sense that the highest cost drivers in medicine are associated with chronic diseases which require medical care over long periods of time, and also may involve expensive hospital visits. Care that is aimed to reduce hospital visits and keep people stable and as well as possible is the objective here. Below is a graph which shows an estimate of the direct and indirect costs for some of the most expensive chronic diseases to manage:
Source: An Unhealthy America: The Economic Burden of Chronic Disease. Milken Institute, Oct. 2007.
Chronic Disease Burden*:
• > 100 million Americans have Diabetes, Kidney Disease, Hypertension, and/or Cardiovascular Disease
• 2 of 3 Americans are overweight; 1 in 5 is Obese
• Chronic diseases account for 96% of Medicare Spending
• Complications from chronic disease account for ~75% of US healthcare spending!
3. End of Life Spending. I wasn't able to find data on % of $ spent on end of life, but I did find the following article on racial differences that indicates between $20k-$30k of spending in the last 6 months of life:
Racial and Ethnic Differences in End-of-Life Costs
Why Do Minorities Cost More Than Whites?
Arch Intern Med. 2009;169(5):493-501.
Background Racial and ethnic minorities generally receive fewer medical interventions than whites, but racial and ethnic patterns in Medicare expenditures and interventions may be quite different at life's end.
Methods Based on a random, stratified sample of Medicare decedents (N = 158 780) in 2001, we used regression to relate differences in age, sex, cause of death, total morbidity burden, geography, life-sustaining interventions (eg, ventilators), and hospice to racial and ethnic differences in Medicare expenditures in the last 6 months of life.
Results In the final 6 months of life, costs for whites average $20 166; blacks, $26 704 (32% more); and Hispanics, $31 702 (57% more). Similar differences exist within sexes, age groups, all causes of death, all sites of death, and within similar geographic areas. Differences in age, sex, cause of death, total morbidity burden, geography, socioeconomic status, and hospice use account for 53% and 63% of the higher costs for blacks and Hispanics, respectively. While whites use hospice most frequently (whites, 26%; blacks, 20%; and Hispanics, 23%), racial and ethnic differences in end-of-life expenditures are affected only minimally. However, fully 85% of the observed higher costs for nonwhites are accounted for after additionally modeling their greater end-of-life use of the intensive care unit and various intensive procedures (such as, gastrostomies, used by 10.5% of blacks, 9.1% of Hispanics, and 4.1% of whites).
Conclusions At life's end, black and Hispanic decedents have substantially higher costs than whites. More than half of these cost differences are related to geographic, sociodemographic, and morbidity differences. Strikingly greater use of life-sustaining interventions accounts for most of the rest.
Author Affiliations: Section of General Internal Medicine, Boston University School of Medicine, Boston, Massachusetts (Drs Hanchate, Kronman, and Ash); Lown Cardiovascular Research Foundation, Brookline, Massachusetts (Dr Young-Xu); and Department of Bioethics, National Institutes of Health, Bethesda, Maryland (Dr Emanuel).
So moving forward, when looking for areas to impact to reduce cost, increase access, and improve quality, the sweet spots are in hospital / provider, chronic disease management, and end of life spending. The type of solutions required will likely be quite different for each. For example, in EoL spending, there are studies showing that Healthcare Directives have had an important effect on reducing EoL spending where they are implemented.
I look forward to exploring each of these areas in detail in future posts.


No comments:
Post a Comment